What could help explain severe coronary disease in someone with a healthy lifestyle who is considered to be at low cardiovascular disease risk? A young man ended up in the ER after a heart attack and was ultimately found to have severe coronary artery disease. Given his age, blood pressure, and cholesterol, his ten-year risk of a heart attack should have only been about 2 percent, but he had a high lipoprotein(a), also known as Lp(a). In fact, it was markedly high at 80 mg/dL, which may help explain it. You can see the same in women: a 27-year-old with a heart attack with a high Lp(a). What is Lp(a), and what can we do about it?
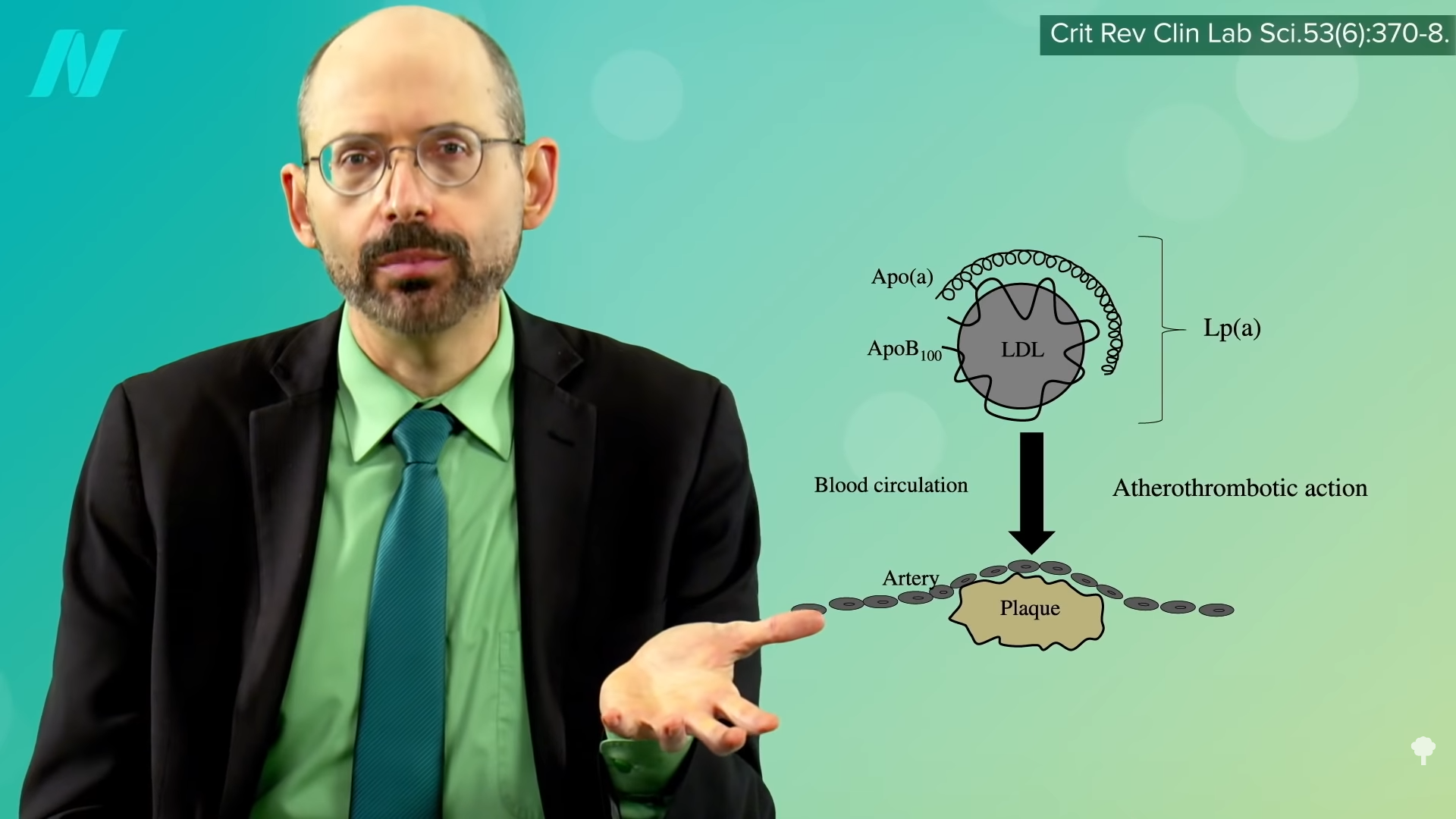
As I discuss in my video Treating High Lp(a): A Risk Factor for Atherosclerosis, Lp(a) is an “underestimated cardiovascular risk factor.” It causes coronary artery disease, heart attacks, strokes, peripheral arterial disease, calcified aortic valve disease, and heart failure. And these can occur in people who don’t even have high cholesterol—because Lp(a) is cholesterol, as you can see below and at 1:15 in my video. It’s an LDL cholesterol molecule linked to another protein, which, like LDL, transfers cholesterol into the lining of our arteries, contributing to the inflammation in atherosclerotic plaques. But “this increased risk caused by Lp(a) has not yet gained recognition by practicing physicians.”
“The main reason for the limited clinical use of Lp(a) is the lack of effective and specific therapies to lower Lp(a) plasma levels.” Because “Lp(a) concentrations are approximately 90% genetically determined,” the conventional thinking has been you’re just kind of born with higher or lower levels and there isn’t much you can do about it. Even if that were the case, though, you might still want to know about it. If it were high, for instance, that would be all the more reason to make sure all the other risk factors that you do have more control over are as good as possible. It may help you quit smoking, for example, and motivate you to do everything you can to lower your LDL cholesterol as much as possible.
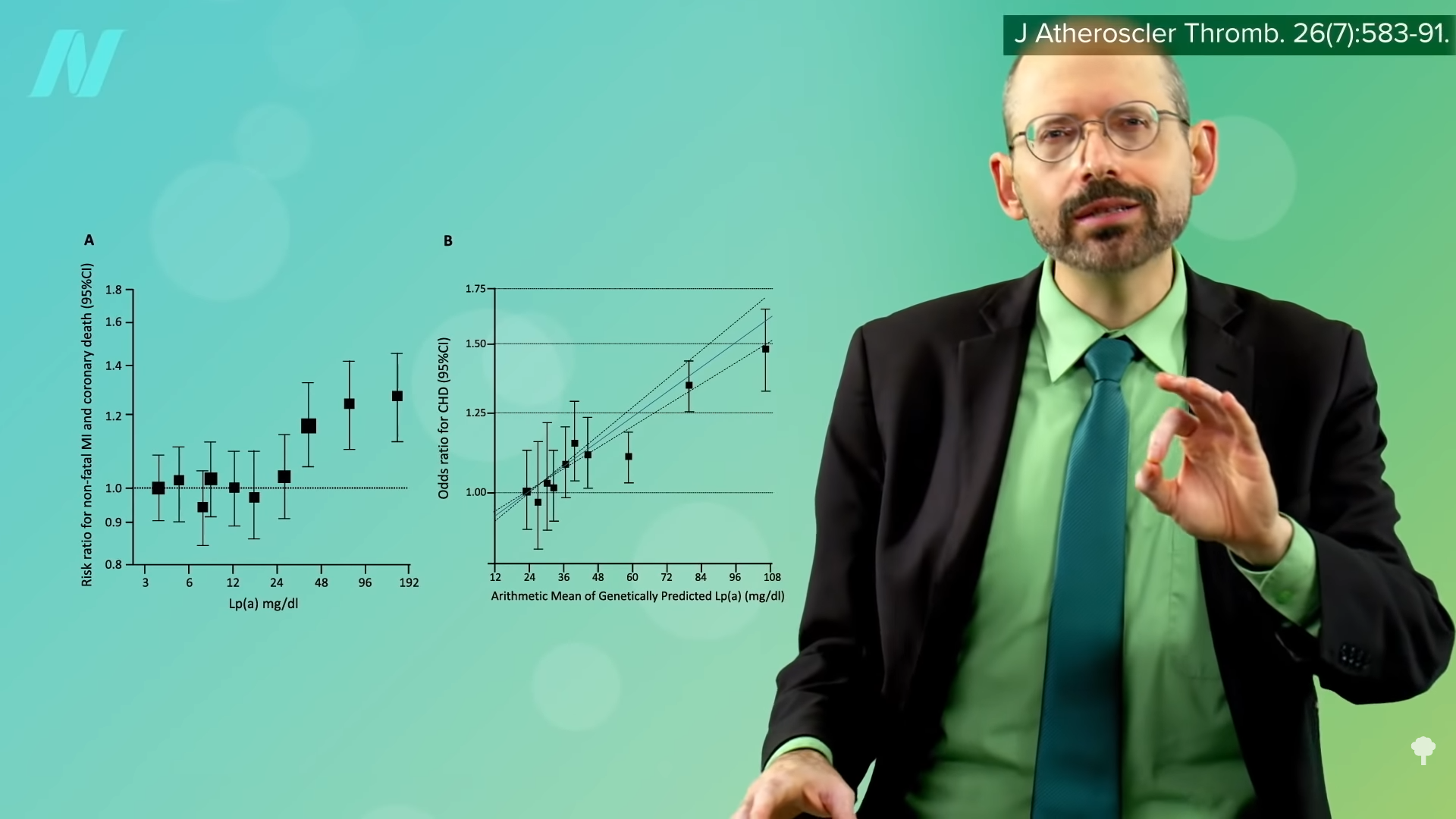
Lp(a) levels in the blood can vary a thousand-fold between individuals, “from less than 0.1 mg/dL to as high as 387 mg/dL.” You can see a graph of the odds of heart disease at different levels in the graph below and at 2:20 in my video. Less than 20 mg/dL is probably optimal, with greater than 30 to 50 mg/dL considered to be elevated. Even when the more conservative threshold of greater than 50 mg/dL is used, that describes about 10 to 30 percent of the global population, an estimated 1.4 billion people. So, if we’re in the one in five people with elevated levels, what can we do about it?
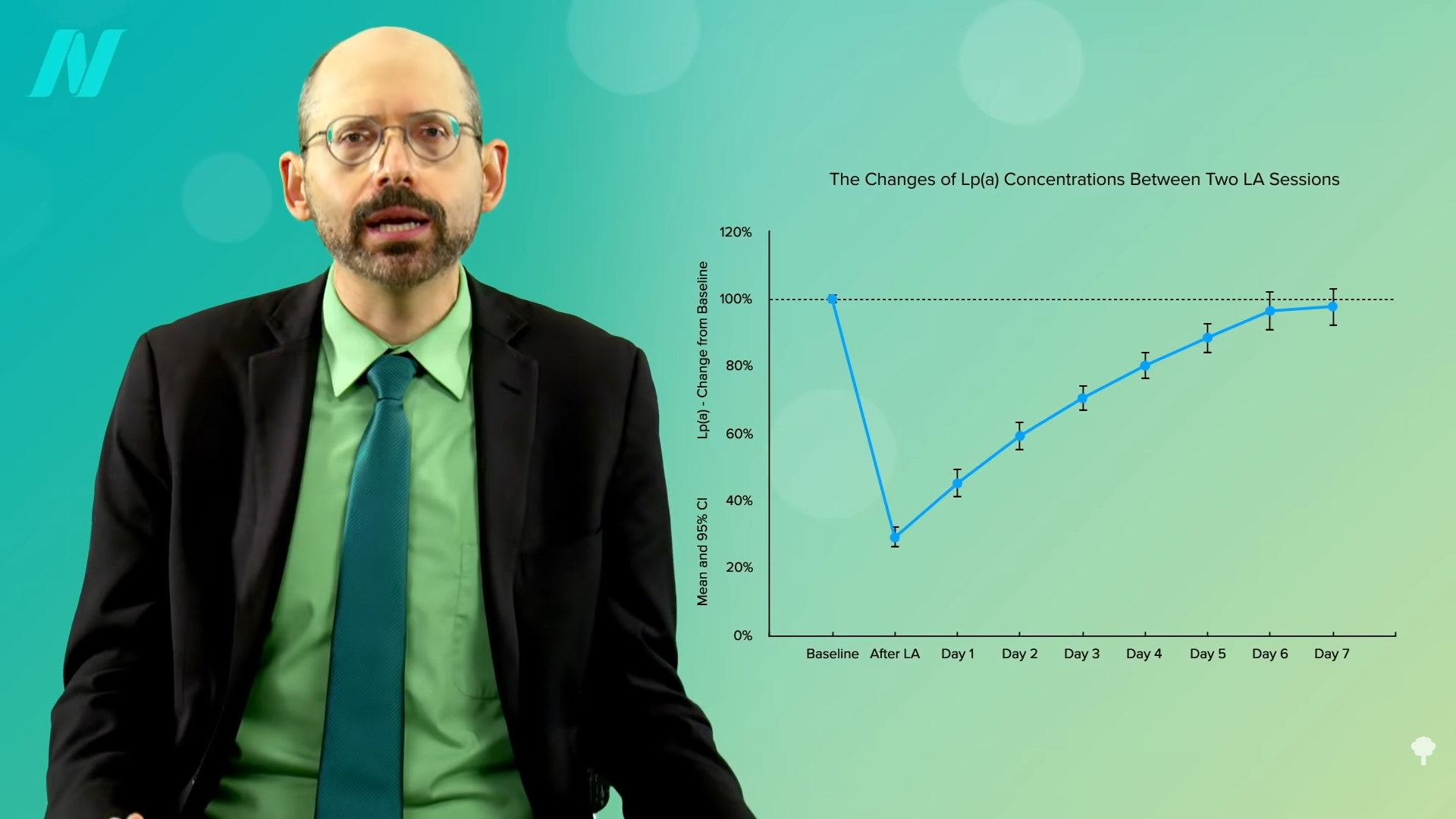
The way we know that Lp(a) causes atherosclerosis is that we can put it to the ultimate test. There is something called apheresis, which is essentially like a dialysis machine where they can take out your blood, wash out some of the Lp(a), and give your blood back to you. And when you do that, you can reverse the progression of the disease. As you can see in the graph below and at 3:06 in my video, atherosclerosis continues to get worse in the control group, but it gets better in the apheresis group. This is great for proving the role of Lp(a), but it has limited clinical application, given the “cost, limited access to centers, and the time commitment required for biweekly sessions of 2 to 4 h each.”

It causes a big drop in blood levels, but they quickly creep back up, so you have to keep going in, as you can see in the graph below and at 3:26 in my video, costing more than $50,000 a year.
There has to be a better way. We’ll explore the role diet can play, next.
I’ve been wanting to do videos about Lp(a), but there just wasn’t much we could do about it until now. So, how do we lower Lp(a) with diet? Stay tuned for the exciting conclusion in my next video.
What can we do to minimize heart disease risk? My video How Not to Die from Heart Disease is a good starting point.


Recent Comments